Fibroids are benign (non-cancerous) growths that can develop in the walls of your womb (uterus). You can have one or more fibroids and they can vary in size. Fibroids can develop on the inside and outside of your womb.
Fibroids are very common. It’s difficult to say exactly how many women have them, as they sometimes have no symptoms, but it’s thought that it’s as many as eight in every 10. Your chance of getting fibroids increases as you get older. They’re linked to your hormones and only develop between puberty and the menopause.
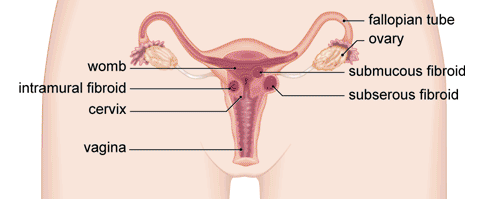
Types of fibroids
There are different types of fibroid, named depending on where they’re growing in your womb.
- Subserous fibroids grow from the outside wall of your womb into the space in your pelvis.
- Intramural fibroids grow in the muscle wall of your womb.
- Submucous fibroids grow from the inner wall of your womb into the space inside your womb.
Subserous and submucous fibroids can grow on a stalk. These are called pedunculated fibroids.
Fibroids usually grow very slowly over years, and new fibroids can continue to develop. Your hormones (oestrogen and progesterone) cause them to grow and develop. When you reach the menopause, they usually begin to shrink as your hormones change.
Symptoms of fibroids
You may not have any symptoms from fibroids, so you may not know you have them. As your fibroids get bigger and you have more of them, they’re more likely to cause symptoms. These include:
- heavy periods that can last a long time – if this happens you can become anaemic, which may cause you to feel tired, dizzy and short of breath.
- swelling in your tummy (abdomen)
- pain and a feeling of pressure in your pelvis
If a fibroid is large and pressing on your bladder or bowel, you may become constipated or feel like you need to pass urine more often. Fibroids are also linked to infertility (not being able to get pregnant) and miscarriage.
Diagnosis of fibroids
Fibroids are sometimes found when you’re having a gynaecological (vaginal) examination for a medical reason, or having investigations to see why you’re not getting pregnant.
Your consultant will ask about your symptoms and your medical history. They will examine your lower abdomen and do a vaginal examination. To do this, your consultant will put gloved, lubricated fingers into your vagina to gently feel for anything different in your womb or cervix. At the same time, they will use their other hand to press on the lower part of your abdomen.
If your doctor thinks you may have fibroids, they may suggest you have further tests. These may include the following.
- A blood test to check if you have anaemia.
- An ultrasound scan. You’ll probably have a scan that looks at your womb from the outside, through your lower abdomen, and from the inside using a device that goes into your vagina. The scan may feel uncomfortable but it shouldn’t be painful.
- A hysteroscopy. A hysteroscopy is a procedure to look inside your womb (uterus). It’s done with a narrow tube-like telescope with a camera called a hysteroscope. Your doctor can take a small sample or tissue (biopsy) at the same time. This can be done with you awake under local anaesthetic or with a short general anaesthetic. Small fibroids in the inside of your womb can sometimes be removed at the same time.
- A magnetic resonance imaging (MRI) scan. A MRI scan can show a lot of detail about your fibroids and can be a useful test to have before surgery.
- This is a test which shows your surgeon what the inside of your abdomen and the outside of your womb look like. A small camera is put into your abdomen through a small cut. As well as looking at your womb, your surgeon can also take samples of tissue (biopsies) to check whether you have fibroids.
Treatment options for fibroids
There are several treatments for fibroids. The treatment that’s best for you will depend on whether you have symptoms, how bad these are, and whether you want to have children in the future.
Your treatment choices will also depend on where your fibroids are, how big they are and how many you have. If you don’t have any symptoms, or if your symptoms are mild, you may not need any treatment. But if you have more severe symptoms, there’s a range of treatment options that may help.
Your consultant will discuss your treatment options with you to help you make a decision that’s right for you. Your decision will be based on your doctor’s expert opinion and your own personal values and preferences.
Medicines
Medicines can’t cure fibroids, but they can help to ease your symptoms. The following types of medicines may help.
- Over-the-counter painkillers. Non-steroidal anti-inflammatory (NSAID) medicines, such as ibuprofen, can help to ease your pain. If you need to take these medicines for a long time, or if they’re not working well enough, see your doctor.
- Medicines that reduce heavy bleeding. These include tranexamic acid, progesterone and levonorgestrel-releasing intrauterine system (an IUS). An IUS is a contraceptive device that goes inside your womb and releases hormones over several years. It can help to reduce the bleeding you have during your period, and it may also help to shrink your fibroids.
- Medicines that shrink your fibroids. Medicines called gonadotropin-releasing hormone analogues (GnRH analogues) can lower your oestrogen levels, which usually shrinks fibroids. If you’re having an operation to remove your fibroids, your doctor may prescribe these for a few months beforehand. As a side-effect, they can give you symptoms similar to the menopause, such as hot flushes and mood swings.
Surgery
There are a number of different operations and procedures that can either treat or remove fibroids. They fall into two groups: those that are an option if you want to have a baby in the future, and those that are an option if you don’t.
If you want to have a baby in the future, your surgeon will suggest a myomectomy. This is an operation to remove your fibroids, but which leaves your womb in place. You can have the operation done through a cut in your abdomen (tummy), or sometimes it may be possible for your surgeon to use keyhole (laparoscopic) surgery.
There is a risk of serious bleeding during a myomectomy. If this happens you might need a hysterectomy, an operation to remove your whole womb. There is also a chance that the fibroids will grow back again. If you don’t want to have a baby in the future, there are several choices. These include the following.
- A hysterectomy. This is an operation to remove your womb. It can be done through a cut in your abdomen, using keyhole surgery or through your vagina. Having a hysterectomy means you will get rid of all your fibroids and they won’t grow back.
- Endometrial ablation. This is a procedure which removes the lining of your womb to reduce heavy bleeding when you have your period. It can treat fibroids on the inside wall of your womb.
- Uterine artery embolisation (UAE). This procedure is where small particles are injected into the blood vessels that supply your fibroids. This blocks the blood supply and the fibroid then shrinks. This can help to ease your symptoms. Because you have your womb, in theory you could get pregnant after it. The effects of the surgery on your fertility or any pregnancy aren’t certain, so, it may be less likely to be used as an option if you want to have a baby.
- Magnetic resonance imaging-guided ultrasound surgery. This is a relatively new procedure, where ultrasound waves are used to destroy fibroids.
Causes of fibroids
Doctors don’t know for sure what causes fibroids. But it’s thought that certain hormones, such as oestrogen and progesterone, may encourage them to grow. You’re more likely to get fibroids:
- as you grow older – your risk increases the closer you are to the menopause
- if you go through puberty at an early age
- if you’re overweight
- if you’re African-Caribbean – women of this background are three times more likely than Caucasian women to get fibroids
- if you don’t have any children
Complications of fibroids
- constipation and problems passing urine, caused by large fibroids pressing on your bladder or bowel
- anaemia, caused by long-term heavy bleeding
- difficulty getting pregnant (infertility)
- difficulties when you’re giving birth to a baby, such as breech position
- fibroids that are on stalks can twist and this can be painful – you may need an operation to remove the fibroid
