An Implantable Cardioverter Defibrillator (ICD) is a small device which can treat people with dangerously abnormal heart rhythms. It sends electrical pulses to regulate abnormal heart rhythms, specifically those that can be dangerous and cause a cardiac arrest.
The heart has an electrical system that regulates the heartbeat. With every heartbeat, there is an electrical signal that follows through your heart, causing it to contract and pump blood. When this process doesn’t happen properly, you could have an abnormal heart rhythm (or arrhythmia) and may need an ICD fitted.
How does an ICD work?
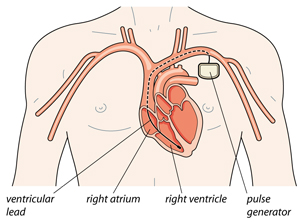
An ICD is placed under the skin to monitor your heart rate, with thin wires connecting it to the heart. An ICD constantly monitors your heart rhythm through the electrodes.
If an ICD notices a dangerous heart rhythm it can deliver one or more of the following treatments:
- Pacing – a series of low-voltage electrical impulses (paced beats) at a fast rate to try and correct the heart rhythm.
- Cardioversion – one or more small electric shocks to try and restore the heart to a normal rhythm.
- Defibrillation – one or more larger electric shocks to try and restore the heart to a normal rhythm.
How is an ICD fitted?
ICDs are inserted under local anaesthetic, but with sedation, so you will feel very sleepy. It can take anything from one hour to three or more hours to implant an ICD, and the time it takes will depend on the type of device you’re having. You will often (but not always) need to stay overnight in hospital and your ICD will be checked thoroughly before you leave.
The ICD is inserted just under your collar bone. It looks similar to a pacemaker and is a little bigger than a matchbox.
- a pulse generator – a battery powered electronic circuit
- one or more electrode leads, which are placed into your heart through a vein.
A different type of ICD is suitable for some people. It’s called a subcutaneous (under the skin) ICD – or SICD for short. An SICD works in the same way as an ICD, but it’s inserted under the skin of the chest (outside of the ribcage) and there are no leads placed into the heart. Your doctor will talk to you about this option if it’s right for you.
Who needs an ICD?
You might need an ICD if:
- you have already had a life-threatening abnormal heart rhythm and are at risk of having it again
- you haven’t had a life-threatening heart rhythm, but tests show you are at risk of one in the future. This is usually because you have inherited faulty genes and may have a condition such as Cardiomyopathy, Long QT syndrome or Brugada syndrome
- you have another heart condition, such as heart failure, and have had or are at risk of having a life-threatening abnormal heart rhythm because of this you have had other treatments to correct your heart rhythm which have been unsuccessful.
How do I live with an ICD?
It’s important to have regular follow-up appointments at your ICD clinic, so you can have your ICD checked. Your appointments may be every 3 to 12 months, depending on the type of ICD you have and if it has delivered any treatment. You’ll need to have follow-up appointments for the rest of your life.
You may have to make some changes to your lifestyle, for instance, if you drive or take part in contact sports. You also need to be aware of how some electronic devices, such as TENS machines or airport security systems, can affect your ICD.
