An Endoscopic Retrograde Cholangio Pancreatogram (ERCP) is a type of x-ray and camera examination that enables your doctor to examine and/or treat conditions of the biliary system (liver, gall bladder, pancreas, pancreatic and bile ducts).
The most common reasons to do an ERCP are jaundice (yellowing of the skin or eyes) or abnormal liver blood tests, especially if you have pain in the abdomen, or if a scan (ultrasound or CT scan) shows a blockage of the bile or pancreatic ducts. Blockages can be caused by stones, narrowing of the bile ducts (strictures), and growths or cancers of the pancreas and bile ducts.
During an ERCP, stents (small plastic or metal tubes) can be inserted into the bile ducts, to allow drainage of bile into the intestine. Stents can also be inserted into the duodenum for patients who have a blockage to the flow of food out of the stomach. An ERCP can give more information about the pancreas and bile ducts, and brushings and biopsies (specimens of cells for analysis) can be taken from the bile ducts or the pancreas.
What happens during the ERCP?
ERCPs are performed by specialist consultants called gastroenterologists. Before the procedure starts, a nurse will attach monitors to one of your fingers to record your pulse and oxygen level, as well as monitors of your blood pressure and heart rhythm. You may be given a local anaesthetic throat spray to help to numb the throat. You will need to lie on your left side and a mouth guard will be placed in your mouth. This enables the telescope to pass through your mouth and oxygen to be administered to you throughout the examination.
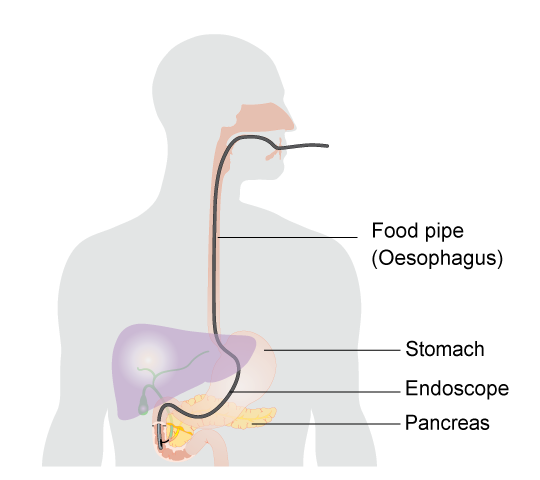
You will be given an injection of intravenous sedation and painkiller through a small needle in the back of your hand or arm. These medicines (known as conscious sedation), will relax you and may make you drowsy but will not necessarily put you to sleep. You will hear what is said to you and be able to respond to any instructions given to you. Once you are drowsy, a flexible tube about the width of an index finger, with a tiny camera on the end of it (duodenoscope) will be passed through your mouth, down your gullet, into the stomach, and then into the top part of the small intestine (duodenum). During the procedure, the consultant will insert a fine wire into the bile ducts and inject dye, which shows up on x-ray. X-rays of various parts of your biliary or pancreatic system will be taken.
If the procedure is being performed to remove stones from the bile or pancreatic duct, a small cut (sphincterotomy) may be made in the lower end of the bile duct to allow a fine tube to pass through. This also allows a small basket or balloon to be inserted to grasp a stone, and for any stones that may get into the bile duct in future to easily pass into the intestine.
Specimens may be taken from the bile ducts using a small brush or forceps, and a plastic or metal tube (stent) may be inserted to help with the drainage of bile or pancreatic juice.
What are the benefits – why should I have an ERCP?
An ERCP allows your consultant to gain detailed and accurate information about your pancreatobiliary system. It often allows treatment of obstructive jaundice (jaundice caused by a blockage in the bile drainage system). It is sometimes used to help remove pancreatic stones or to put a stent into a narrowed pancreatic duct. This can be helpful in dealing with pain.
What are the risks?
ERCP is generally safe but complications can sometimes occur.
Minor complications:
- Mild discomfort in the abdomen and a sore throat, which may last up to a few days
- Loose teeth, crowns and bridgework can be dislodged, but this is rare
- Mild inflammation of the pancreas (pancreatitis). This can happen in approximately five in 100 people. If pancreatitis happens, you will have pain in the abdomen, usually starting a few hours after the procedure and lasting for a few days. The pain can be controlled with painkillers and you will be given an intravenous (into a vein) infusion of fluids in hospital to keep you hydrated until the pain subsides
- Inability to gain access to the bile or pancreatic ducts
- Irritation to the vein in which medications were given is uncommon, but may cause a tender lump lasting for a couple of days
Possible major complications:
- Severe pancreatitis can occur following an ERCP. We can treat this with medication or surgery. Although it is very rare, severe pancreatitis can be fatal (less than one in 500 cases).
- If sphincterotomy (a small cut in the bottom of the bile duct) is performed, there is a risk of bleeding which usually stops quickly by itself. If it does not stop by itself we may inject you with adrenalin through the endoscope. However, in severe cases, blood transfusion, a special x-ray procedure or an operation may be required to control the bleeding.
- Very frail and/or elderly patients can get pneumonia from stomach juices getting into the lung (approximately one in 500 cases)
- A hole may be made in the wall of the duodenum (perforation), either as a result of sphincterotomy or due to a tear made by the endoscope. This happens in less than one in 750 cases.
- A very rare complication is a reaction to one of the sedative drugs used
Although ERCP carries risks, it is only carried out when the doctors have carefully balanced the risks of doing this test compared with doing any other test or operations, and the risks of doing nothing. Your consultant will be happy to discuss this with you further.
Preparing for the ERCP
Before you have the ERCP, blood tests will be taken to check the clotting of your blood and your blood count. In order for the doctor to be able to have a clear view with the camera, it is important that you do not eat or drink anything for six hours before the test. You will usually be given an oral dose of antibiotic about an hour before the ERCP which you can take with a small amount of water.
If you are taking any blood thinning medicines (e.g. warfarin, rivaroxaban, aspirin, clopidogrel), please speak to your consultant, as you may need to stop these prior to your ERCP. Also, please inform your consultant if you are a diabetic.
The Procedure
The actual procedure lasts between 15 minutes and one and a half hours, but half an hour is an average time.
You may experience some mild stomach cramps from the air that was introduced into your stomach during the procedure. These will soon disappear. We will give you pain killing suppositories (into your back passage) before the end of the procedure to prevent pancreatitis.
Afterwards, simple pain killer tablets, e.g. paracetamol, may be taken. Taking peppermint (e.g. as peppermint tea or peppermint water) can help to pass the air.
If you develop severe abdominal pain, please inform your consultant immediately. If you have gone home, consult your GP or go to the nearest A&E department.
The nurse will monitor your pulse and blood pressure regularly and observe you for any complications. Most complications become apparent within six hours of the procedure, so you will remain under observation for that time.
You will need to stay in the Endoscopy Unit until you are fully awake, which usually takes at least one hour and under observation for six hours after the procedure. When going home after your procedure, you will need to be escorted home by a responsible adult.
Most of the time, you can eat as normal once you are fully awake. However, depending on the type of treatment you had during the procedure, you may be asked to fast (not eat anything) for 12 hours or more afterwards.
You should continue to take your usual medications, unless we tell you otherwise. If you have been asked to stop any medicines before the procedure, we will confirm when to restart these before you leave Endoscopy. The effect of the sedative can last up to 24 hours so you should not drive, operate machinery or drink alcohol during that time.
Your consultant or nurse will talk you through the results of the procedure, but sometimes you may be sleepy and not be able to remember the details. The results will be sent to your referring doctor.
