People often confuse the terms tendonitis, tendinosis, and tendinopathy. These terms, along with paratenonitis, tendon rupture, and partial tendon rupture, describe a variety of tendon conditions, including inflammation, degeneration, and injury.
Tendons are the fibrous tissues that connect muscle to bone, and there are hundreds of tendons throughout the body. Certain tendons are more prone to problems than others. For example, many people have strained an Achilles tendon at one point or another. Moreover, a single tendon can have more than one problem at a time.
When the tendon tears it is called a rupture. If a tendon is torn in two pieces it is called a complete rupture, and if some of the tendon still remains intact it is called a partial rupture.
While most experts define tendinopathy as an umbrella term to describe all tendon conditions, others may use it to describe a chronic tendon condition that fails to heal. For example, a runner who has suffered a hamstring tendon rupture that does not heal properly may be diagnosed with tendinopathy.
Knee
Patellar tendinopathy is a change in the quality of the tendon that joins your kneecap (patella) to your shin bone (tibia). The tendon weakens, becomes painful and is less able to cope with the mechanical loads you put on it during exercise. Patellar tendinopathy is also called ‘jumper’s knee’ because the injury commonly occurs during jumping sports such as basketball, netball or volleyball. It’s also sometimes referred to as patellar tendonitis.
The main thing you’ll notice is pain at the bottom edge of your kneecap, or just below it. This usually comes on gradually rather than suddenly. When you first get the pain it will probably only come after you exercise. As time goes by you may get the pain during exercise, perhaps reducing after you warm up. This may then develop into constant pain during activity. If you don’t have treatment for patellar tendinopathy there’s a possibility that your tendon will eventually tear (rupture). Your performance may be unaffected by patellar tendinopathy at first, but as the condition worsens you’ll find you’re not able to perform so well. As well as having pain, the painful area of your knee may be tender to the touch, especially when your leg is straight. You may also have stiffness or tightness around your knee in the morning that eases as you start to move around.
Doctors aren’t exactly sure why patellar tendinopathy happens. It’s an overuse injury which is often seen in athletes who jump, but it can affect anyone. It’s believed to be caused mainly by repeated stress on the patellar tendon when you do sports which involve jumping. Jumping and landing cause repeated strain to the patellar tendon resulting in changes to its cell and protein structure.
You may be more likely to get patellar tendinopathy if you’re aged between your teens and thirties, although it can happen in older people. It has been linked with overtraining, or playing on hard surfaces. Some studies have found that jumper’s knee is more common in taller and heavier people.
There’s no quick fix for patellar tendinopathy. You may need a long period of rehabilitation before your symptoms go completely. However, the earlier you get treatment, the quicker and better your recovery is likely to be.
Achilles (Ankle)
Achilles tendinopathy is injury to the band of tissue (tendon) that runs down the back of your lower leg to your heel. You may get pain, stiffness and sometimes swelling that makes it difficult to move freely.
Achilles tendinopathy can make it hard to walk and may stop you carrying on as normal. It can affect anyone, but particularly people who do activities that involve running and jumping. It’s thought that around 150,000 people are affected by Achilles tendinopathy every year.
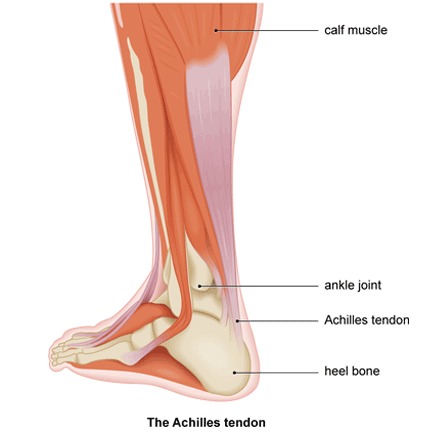
Tendons help bones and joints to move when your muscles contract. Your Achilles tendon is the thickest tendon in your body and is very strong and flexible. It connects your calf muscle to the bone in the heel of your foot. This enables you to go on tiptoe or move forward when you walk, run or climb.
You can get Achilles tendinopathy through a specific injury or by overuse. The tendon can deteriorate gradually over a period of time.
The main symptoms of Achilles tendinopathy are increasing pain and stiffness, usually at the back of your ankle. You may also notice some swelling. This is sometimes called tendonitis.
Your Achilles tendon might feel tender when you touch it. There may be a grating noise or creaking feeling (crepitus) when you move your ankle.
The pain can come and go. It may be worse first thing in the morning or after you’ve done any exercise or activity. Your Achilles tendon may feel particularly stiff when you first get up or if you haven’t moved for a while. The stiffness may ease off when you start moving again.
Achilles tendinopathy can interfere with your day-to-day life. It may mean you need to take time off work or studies. You may not be able to do so much activity, including sports, but talk to a physiotherapist about this for advice.
Sudden pain in your heel or calf, which quickly becomes swollen, bruised and sore, can mean you’ve torn the tendon. You may actually hear it snap.
Achilles tendinopathy gets worse over time if not treated. It’s usually caused by overusing your Achilles tendon. Very small tears can start to develop. Without treatment, these won’t heal and your tendon can become weaker.
Age makes Achilles tendinopathy more likely. As you get older, your Achilles tendon becomes less flexible and less able to cope with strain on it. People over 60 are more prone to tendon damage.
Your overall health and fitness can be another cause. You’re more at risk of Achilles tendinopathy if you:
- have a family history of the condition
- have a history of tendon or muscle injury
- have a health condition such as arthritis, diabetes or high blood pressure
- are obese
- have high cholesterol levels
- take an antibiotic belonging to the quinolone group
Your feet and the way you walk make a difference too. Wearing the wrong sort of shoes, or ones that don’t fit properly are both bad news for your Achilles tendon. Continual wearing of high heels is not good for the Achilles tendon.
You may have ‘flat feet’ with arches lower than they should be. These can make your whole foot roll inwards when you walk or run. This is called over-pronation and can contribute to Achilles tendinopathy. High-arched feet can cause problems as well.
Sports and other activities can put a lot of stress on your Achilles tendon. Running is the biggest risk but anything that involves jumping – like dancing, tennis or basketball – may damage your tendon. Extra problems can be caused by:
- poor equipment, including inappropriate footwear
- poor technique, like suddenly increasing how much exercise you do
- poor posture or alignment
- hard, slippery or high-friction surfaces
- extreme weather conditions, particularly the cold
Surgery may be an option if other treatments haven’t worked after several months, especially if your symptoms are seriously affecting your everyday life.
The operation may involve removing damaged areas of your tendon and repairing what’s left. The surgeon may need to use tissue from higher up your Achilles tendon, or from another of your tendons, to do these repairs. The wound may take time to heal and leave scars.
